
Our emergency care resource for Epidermolysis Bullosa (EB) offers vital information for handling sudden illness or injury effectively in individuals with EB.
This comprehensive guide, created in partnership with Cincinnati Children's, is designed to support medical staff, patients, and families in emergency situations and upcoming surgeries, ensuring prompt and informed care during critical moments. Navigate to a specific section by clicking the links below:
Clinical Essentials: Understanding EB Types
Epidermolysis Bullosa (EB) is a rare and complex genetic disorder affecting the skin and oral mucosa, with potential involvement of the esophagus, eyes, urethra, and potential complications in other internal organs. EB encompasses several distinct types, each characterized by a spectrum of symptoms that may overlap while also presenting unique clinical features. Among these types are:
- Dominant Dystrophic Epidermolysis Bullosa (DDEB)
- Recessive Dystrophic Epidermolysis Bullosa (RDEB)
- Epidermolysis Bullosa Simplex (EBS)
- Junctional Epidermolysis Bullosa (JEB)
- Kindler Syndrome
These classifications may help medical professionals treat their patients with EB, emphasizing the need for tailored management strategies. There are in fact over 30 subtypes of the disease. While every patient is unique, understanding the specific EB type, if possible, can inform personalized care. Refer to the patient's EB Wallet Card or inquire with the family for the patient's EB type.
Emergency Management
Extreme Skin Fragility
- May use silicone-based dressings or non-adherent dressings
- Avoid adhesives and tape. Do not rub or create friction (dab instead)
- Never slide or grab; move by lifting body parts from below
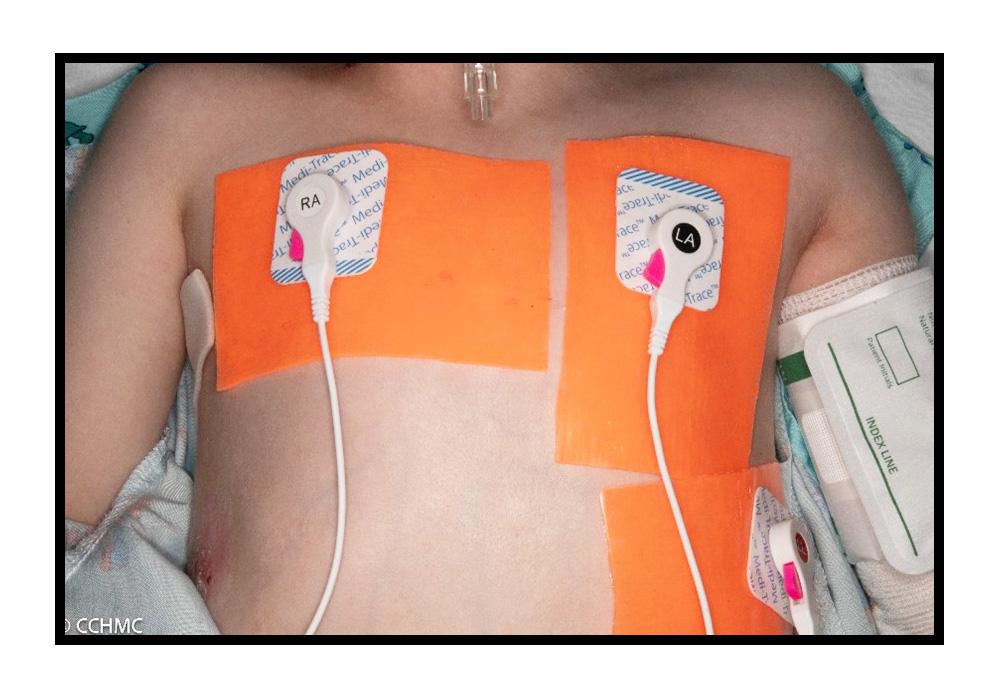
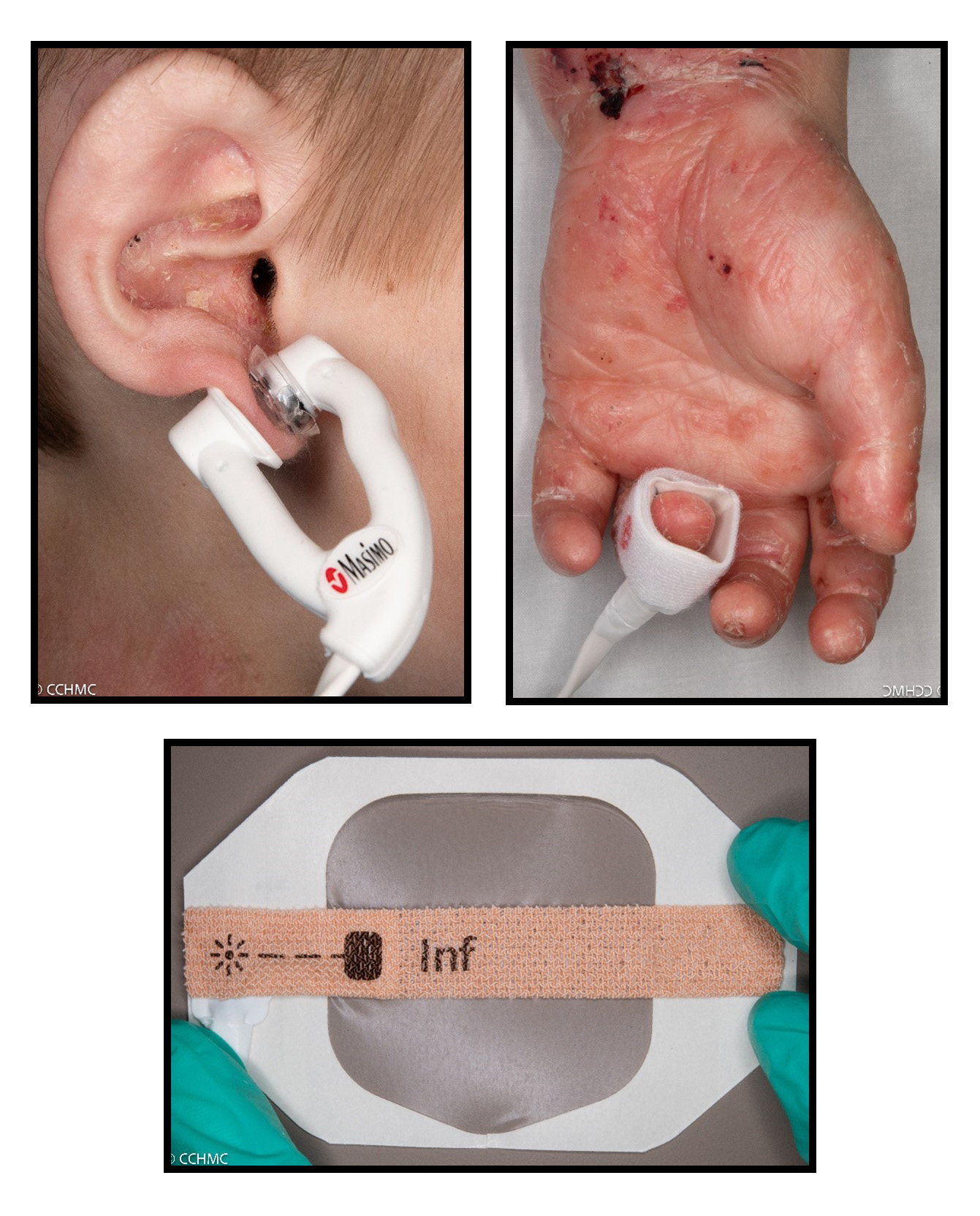
- Remove adhesives from EKG leads and pulse ox (may secure with silicone-based or non-adherent products)
- Apply roll bandaging to pad the extremity before applying blood pressure cuff
- In an incident where adhesives have been applied, leave in place until patient is stable. Use adhesive removal spray or emollient to gently loosen and carefully remove adhesives to minimize trauma. Alternatives include Vaseline®, mineral oil, coconut oil, normal saline, baby oil, or tap water
- Tolerance with blood pressure monitoring may vary.
- Discuss the preferred extremity with the patient in order to avoid wounds or unnecessary skin trauma.
- The blood pressure cuff may be applied over clothing or overtop an extremity covered with roll gauze to reduce shearing of the skin.

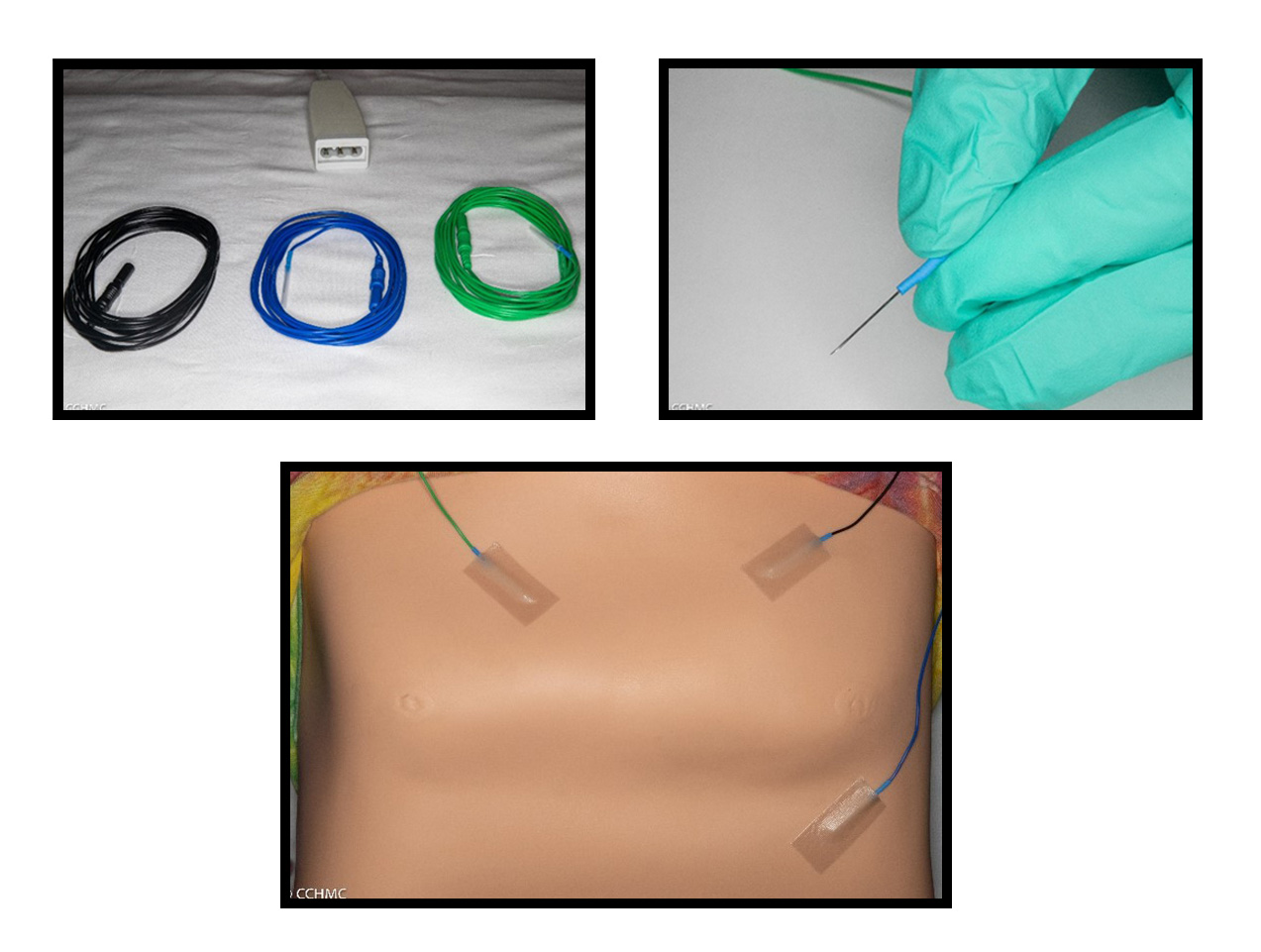
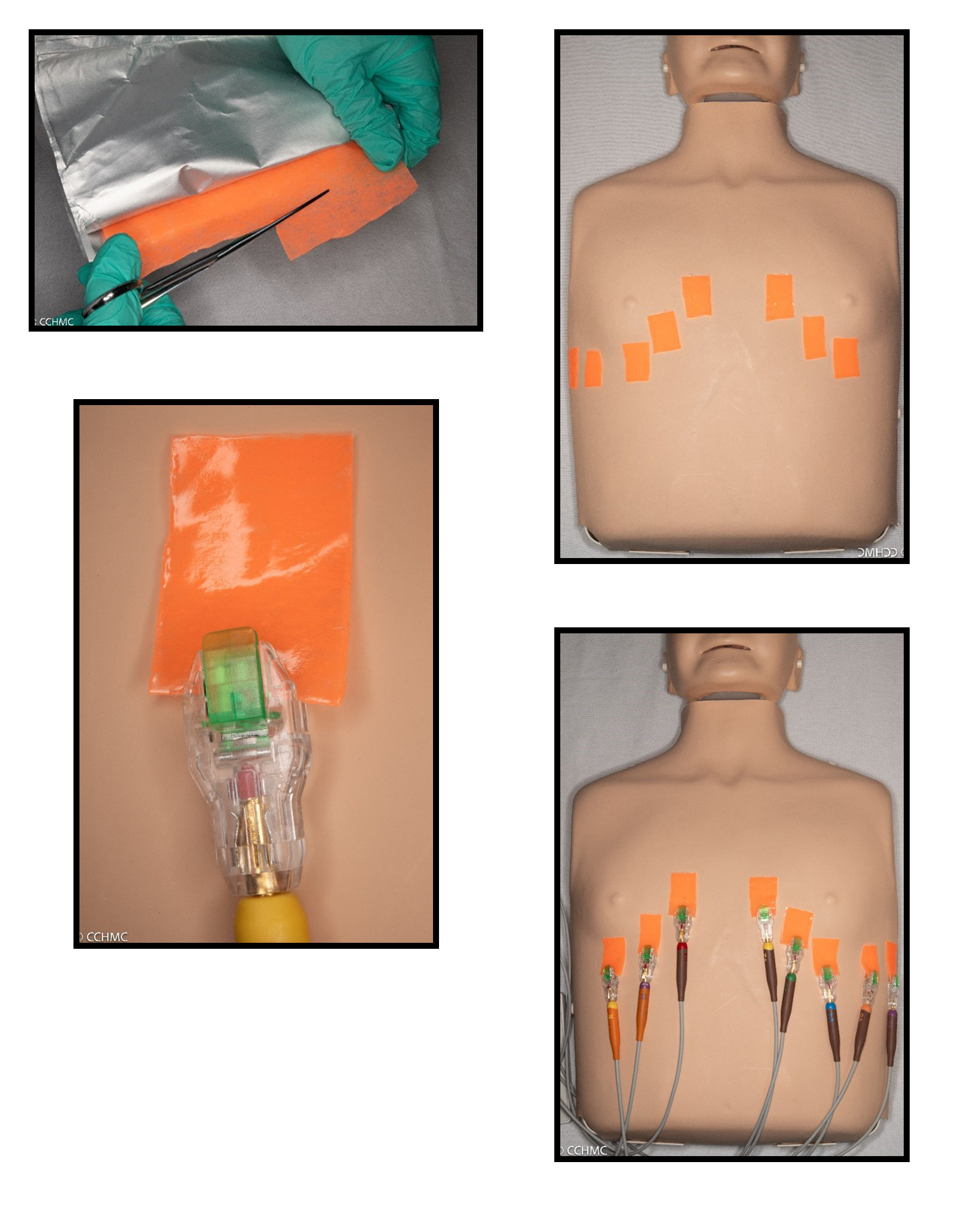
Multiple techniques can be considered for cardiac monitoring. Techniques may include: removing adhesives from EKG leads and securing with silicone-based tape, applying EKG leads directly to a non-adhesive gel defibrillator pad, utilizing needle electrodes or covering EKG leads with ultrasound gel and securing with silicone-based tape or by applying EKG clips directly to non-adhesive gel defibrillator pads.
Use of non-adhesive gel defibrillator pads:
Needle Electrodes:
EKG Leads with ultrasound gel:
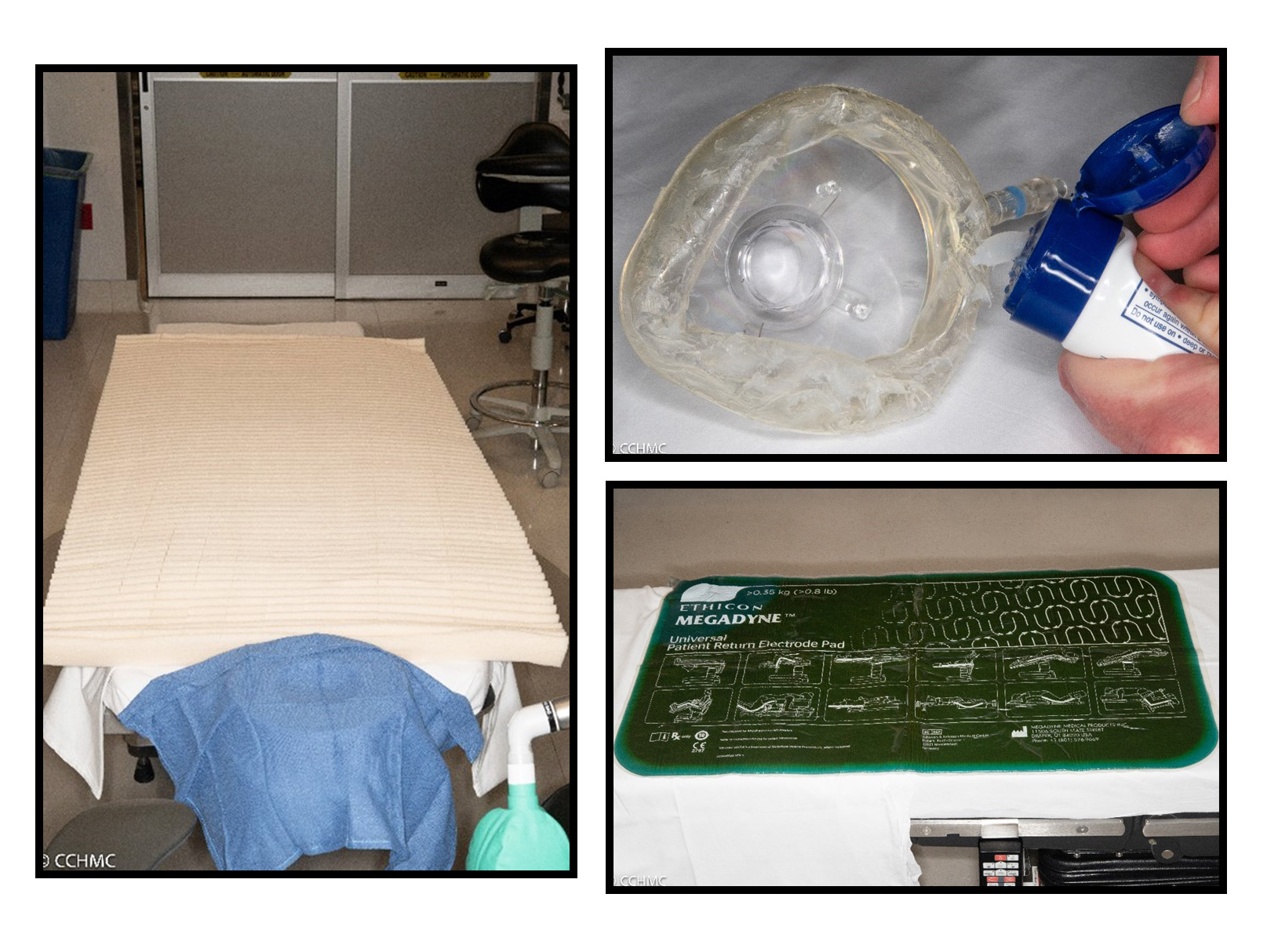
Apply a liberal amount of ultrasound gel to the EKG pad to cover the adhesive then secure to the skin with a silicone-based tape. If silicone-based tape is not tolerated, cover the chest with a towel to keep the leads adherent to the chest.
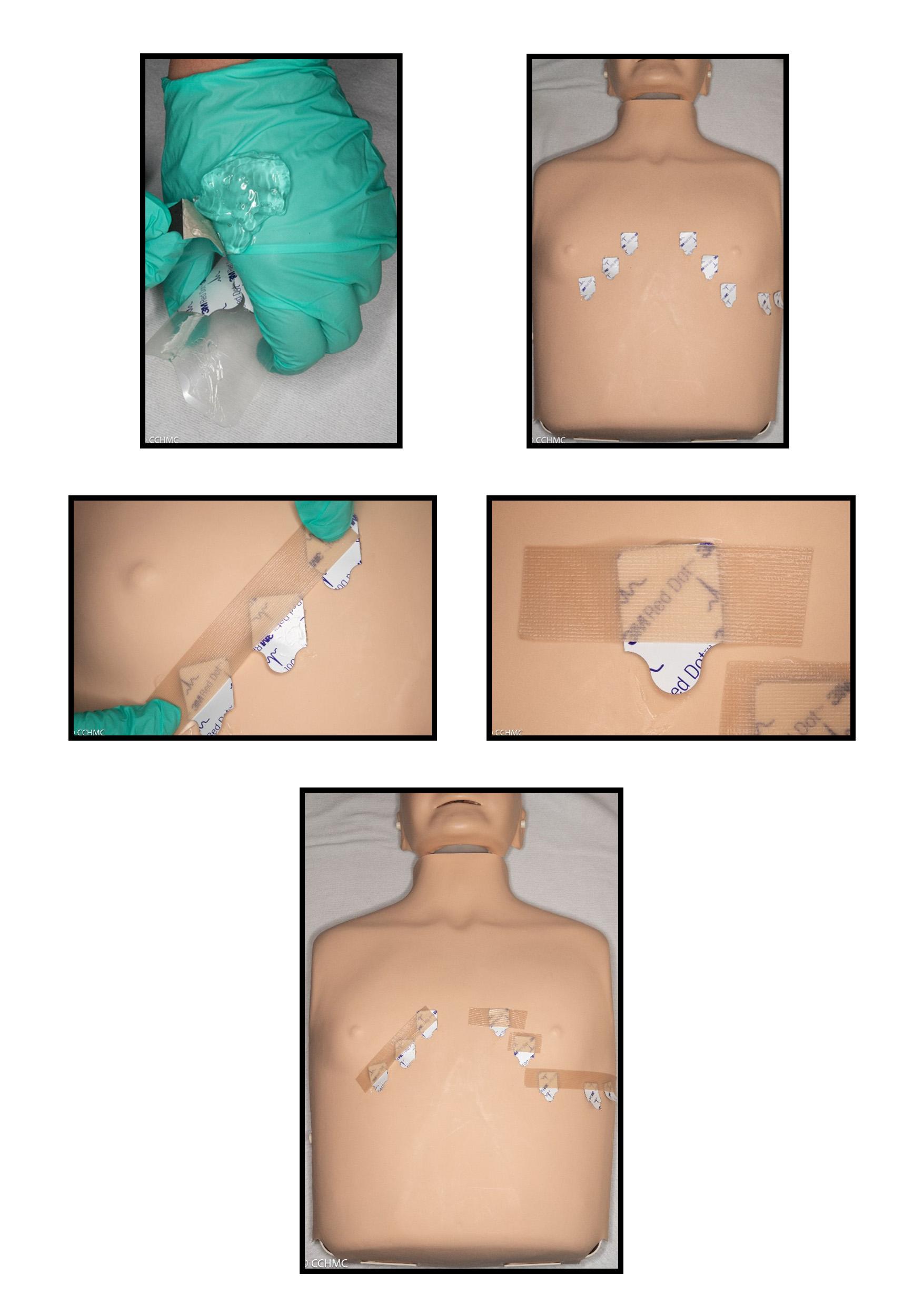
EKG with non-adhesive gel defibrillator pads:
Cut non-adhesive gel defibrillator pads down to size, apply to the chest and clip the EKG clips directly to each defibrillator pad.
Multiple techniques can be considered for pulse oximetry monitoring. Techniques may include: utilizing a Velcro or clip pulse ox; removing the pulse ox adhesive and securing with silicone-based tape; placing a silicone contact layer dressing beneath the pulse ox or EKG leads; or covering the pulse ox adhesive with Tegaderm without exposure of adhesive and securing the pulse ox with tape while avoid contact with the skin.
Physical Exam
- Keep in mind that modifications may be required for routine exams.
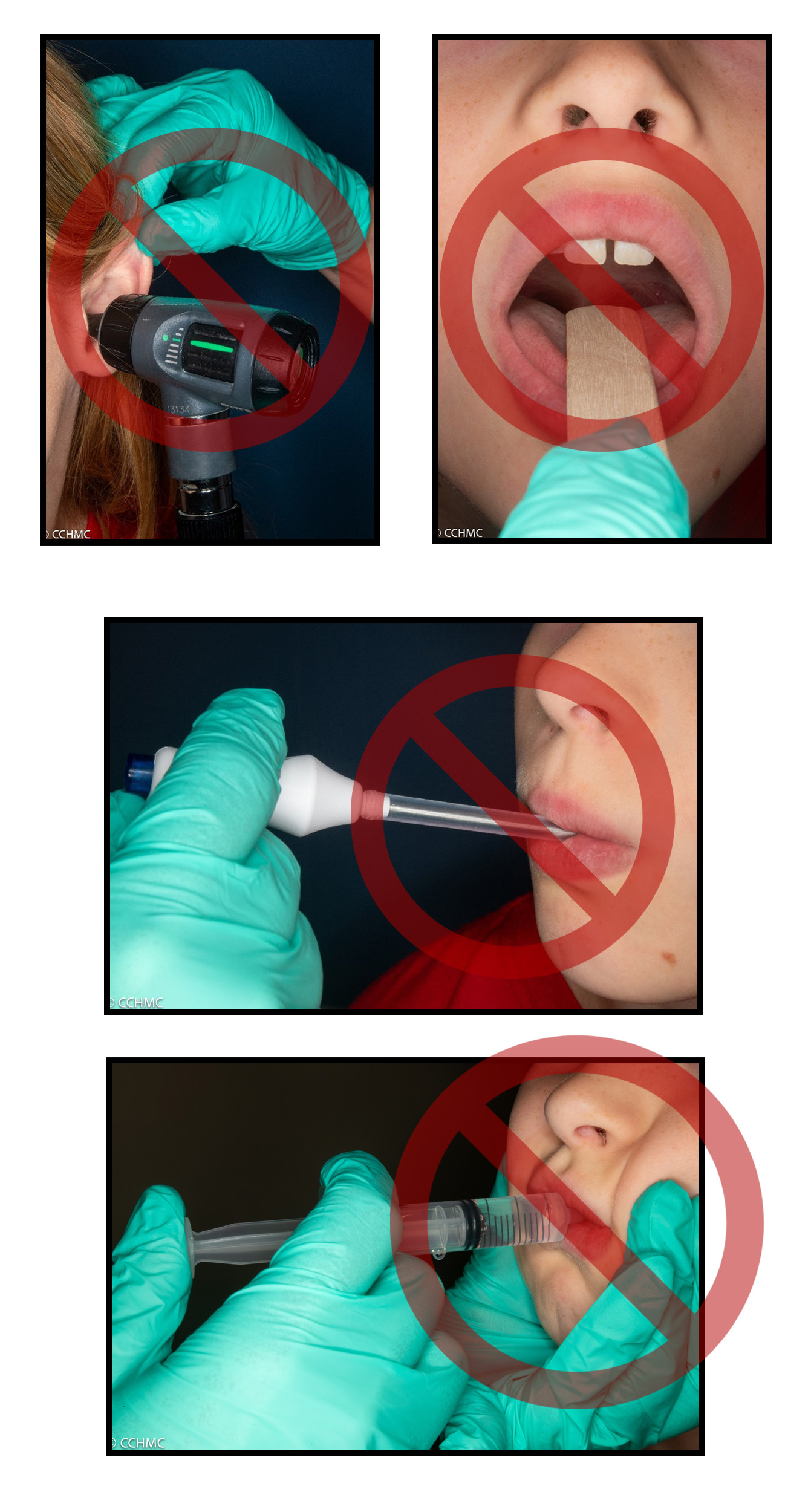
- Avoid pulling or manipulating the ear lobe to prevent trauma.
- Avoid using a tongue depressor to visualize the oral cavity.
- Consider using a temporal thermometer since the tongue may be scarred to the floor of the mouth and axillary wounds may be present. Rectal temperatures are not preferred, but, if necessary, liberal lubrication should be applied to the probe.
- Avoid pinching the cheeks for medication administration.
- Palpation and auscultation of the chest and abdominal should occur with light pressure and avoidance of friction and rubbing.
Utilizing EB-friendly dressings during skin preparation in hospital settings is crucial for individuals with EB. These specialized dressings minimize trauma and friction on fragile skin, reducing the risk of blistering and wound exacerbation. By prioritizing EB-specific care, medical professionals can ensure safer procedures for patients with this condition. Examples include:
- Dressing supplies tolerance varies among individuals and no two patients are the same.
- Refer to the patient and/or family for skin care recommendations.
- Generally, silicone-based products are well tolerated by individuals with EB.
- If an adhesive product is incidentally applied to the skin, gentle loosen and remove with an adhesive remover spray, coconut oil or emollient.
- debra of America's essential guidance on basic EB care:
- International Consensus - Best Practice Guidelines for Skin & Wound Care in EB
- This article refers to wound care management and dressing supply recommendations for EB types, including specific considerations for neonates, intra-operative care, gastrostomy tube care and trach care. Information is also provided for wound care recommendations for infection, moisture, debridement, squamous cell carcinoma, etc.
- Skin and Wound Care: Patient Guide
- This reference by DEBRA International provides information on blister management, management of different types of acute and chronic wounds, dressing types, factors affecting wound healing, infection prevention and management, odor control, itch control and identification of squamous cell carcinoma.
Anesthesia/ENT Airway Alert
- EB related challenges include: difficult airway due microstomia and poor mouth opening, skin and mucous membrane fragility, difficult IV access and securement, and risk of anemia, cardiomyopathy and aspiration
- Consider fiberoptic intubation
- Use fiberoptic bronchoscope or well-lubricated laryngoscope w/ smaller than expected ETT if length appropriate
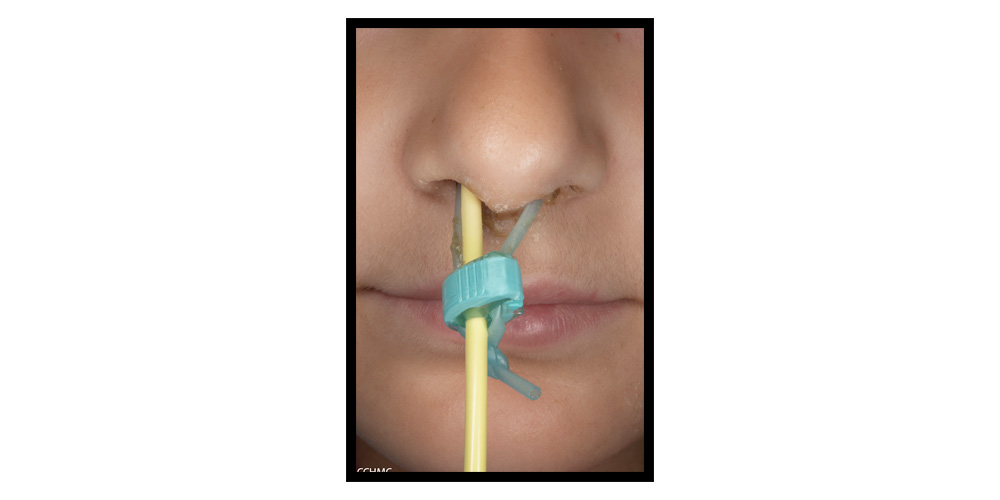
- Non-invasive airway management preferred. Nasal cannula or emollient on face mask with silicone-based dressing as barrier on skin to reduce trauma
- Recommend padding the jawline with silicone foam for jaw thrusts
- Prepare for difficult intubation with ENT/Pulmonary back-up
- Difficult intubation should be anticipated in all EB patients.
- Airway management in EB patients can be challenging and hazardous due to the risk of edema, blistering, and bleeding of friable tissues.
- May be conventionally intubated, but fiber-optic intubation should be strongly considered, with careful tube securing without adhesives.
- Supraglottic airways may be considered, with attention to device selection and lubrication to minimize trauma.
- Video laryngoscopy can be successful but requires careful technique and lubrication of equipment.
- Emergent surgical airway equipment should be readily available.
- Safe for subcutaneous or intramuscular injections.
- Please refer to Additional Resources and References below for up-to-date publications on anesthesia and airway management.
Intraoperative Face Protection
- Apply silicone-based products to the face and jawline to prevent skin trauma.
- Extra padding may need to be applied to the jawline to reduce trauma during jaw thrusts which is a commonly seen occurrence.
- Individuals with EB are at increased risk of intraoperative corneal abrasions therefore preferred eye protection should be discussed with the patient. Eye precautions may include: taping the eyelids closed with a silicone-based tape, placing saline soaked sterile gauze over the eyes or frequent application of eye lubricating drops or gel.

- Intraoperative fluid therapy should focus on maintaining euvolemia and replacing blood loss.
- Excessive crystalloid administration should be avoided to prevent complications such as hypervolemia and impaired wound healing.
- A balanced electrolyte solution is recommended until a transfusion threshold is met, particularly in patients with cardiomyopathy or renal failure.
- Goal-directed fluid management guided by invasive monitoring is advised in cases of significant blood loss or fluid shifts.
- Emergence and tracheal extubation should occur in a controlled environment with difficult airway equipment readily available.
- Smooth emergence with minimal coughing and patient movement is ideal to prevent blister formation or airway bleeding.
- High-flow nasal cannula or lubricated anesthesia circuit facemask can provide supplemental oxygen post-extubation.
- Perioperative Recommendations for Anesthesia Care for Patients with Epidermolysis Bullosa
- These recommendations were written by anesthesiologist, Dr. Eric Wittkugel and Dr. Abigail Monnig, with Cincinnati Children’s Hospital Medical Center. These recommendations include information regarding pre-operative assessment, EB-related body system involvement, common surgical procedures, general management, suggested supplies, anesthetic techniques, emergence/post-operative care and surgical considerations.
- Anesthetic Management of Children with Epidermolysis Bullosa
- This article reviews anesthesia pre-operative, intra-operative, and post-operative care as well as monitoring and analgesia.
- Anesthetic Management of Adults with Epidermolysis Bullosa
- This article reviews anesthesia pre-operative, intra-operative and post-operative care of adults with EB.
- Anesthetic Management and Outcomes of Patients With Epidermolysis Bullosa: Experience at a Tertiary Referral Center
- This article provides recommendations for a standardized clinical care pathway to minimize perioperative adverse events. This retrospective chart review includes EB patient demographics, anesthetic methods, perioperative outcomes and adverse events at Children’s Hospital Colorado with the utilization of a standardized clinical care pathway.
- [VIDEO] Anesthesia Management and Outcomes in Patients with Epidermolysis Bullosa - By Dr. Melissa Brooks Peterson, MD
- This 45-minute video by anesthesiologist, Dr. Melissa Brooks Peterson, discusses EB anesthesia care and outcomes.
- Neonatal Epidermolysis Bullosa: A Clinical Practice Guideline
- This Clinical Practice Guideline has EB recommendations for skin care and management and medical care that overlaps with general EB care. Refer to Appendix 5 for the Neonatal EB Hospitalization Implementation with photographs of ETT securement, mask ventilation and nasal cannula oxygen delivery.
Intravenous (IV) and Central Line Access
-
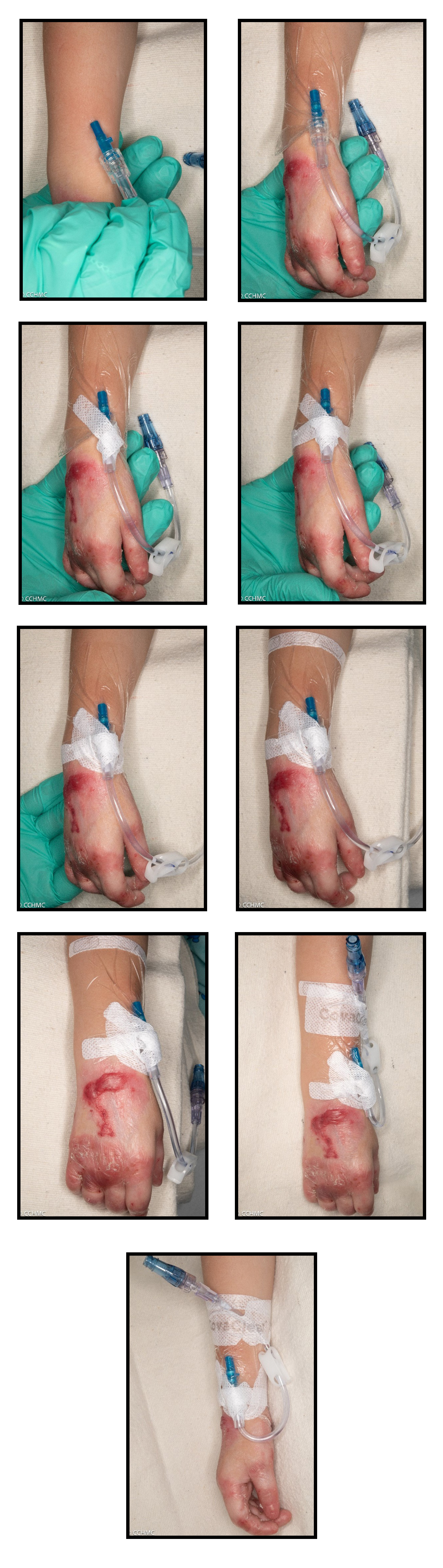
Refer to fragile skin dressing for IV placement
- Dab, do not rub, skin with alcohol pads for labs/IV/antiseptic cleansing
- May require ultrasound for IV placement
- Consider topical lidocaine cream prior to IV placement
- If EB safe IV products are not accessible for IV placement, consider consulting with patient or family for recommendations for products.
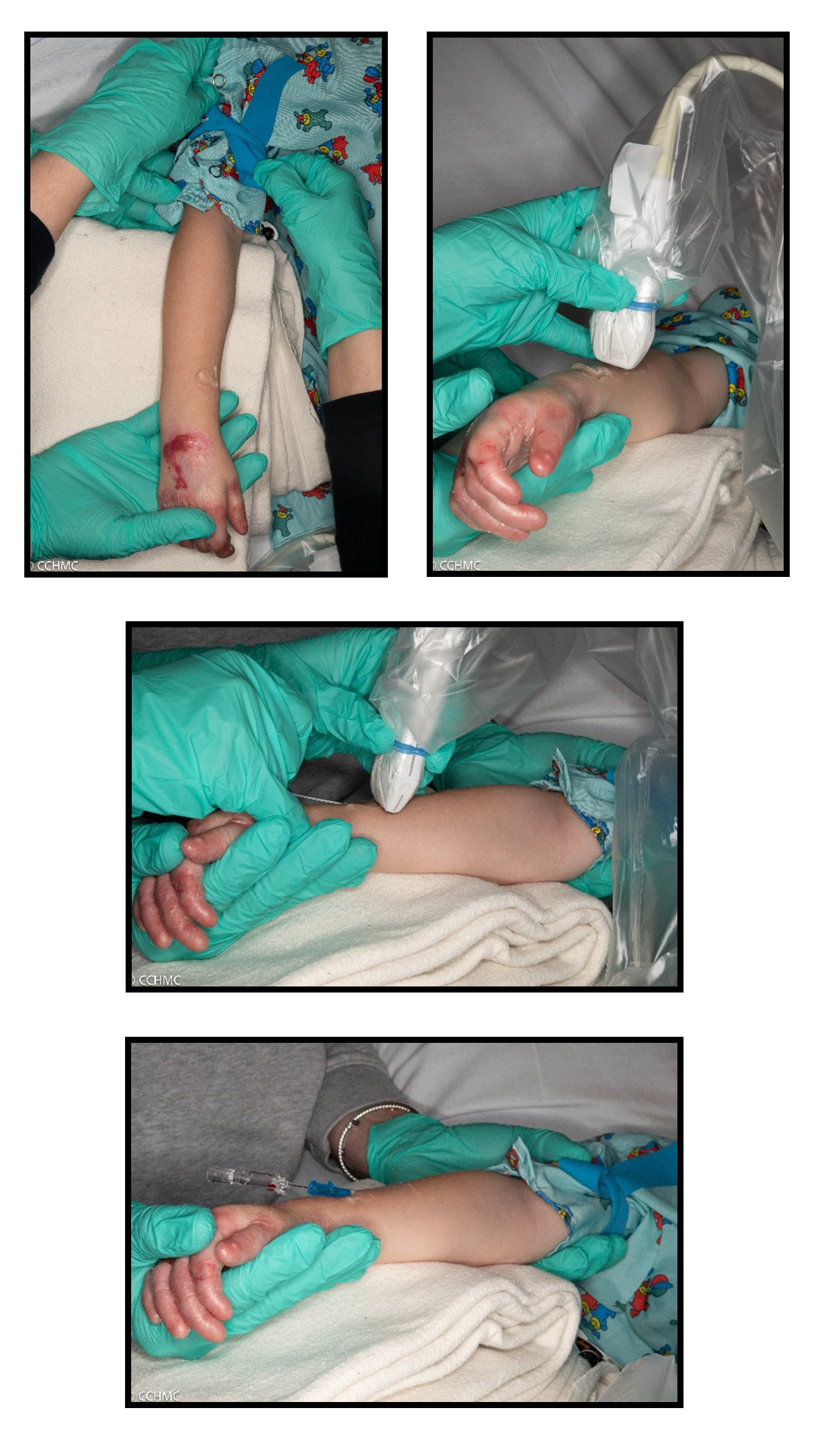
- Intravenous access can be challenging and may require ultrasound guidance
- Gentle manual pressure should be applied to distend the vein, or gently apply tourniquet over clothing and inflate manual BP as tourniquet
- Once access is established, secure the catheter hub with non adhesive dressing or soft silicone tape, wrapping it with self-adherent wrap or gauze
Intravenous Access:
- Obtaining intravenous access may be difficult and require the use of ultrasound-guided placement.
- If desired, an topical anesthetic cream may be applied prior to insertion to aide in pain reduction.
- A touriquent may be gently applied over clothing, light pressure may be applied with the hands to distend the vein or a manual blood pressure cuff may be inflated to act as a touriquent.
Ultrasound guided IV insert:
Central Line Fragile Skin Dressing for EB Patients PDF
Novel Approach to Catheter Securement with silicone-based clear IV dressing
- Diagnosis and Care of the Newborn with Epidermolysis Bullosa
- Refer to this article for a diagram demonstrating a fragility skin IV dressing.
Catheters and Tubes
- Avoid invasive catheters and NG placement if possible;
- Clean catch urine samples are preferred;
- If urinary drainage is needed, consider smallest effective size with indwelling urinary catheter favored over intermittent catheterization;
- If catheter or tube is needed, insert carefully with extra lubrication.
- If an NG tube is indicated, consider placing a nasal bridle or securing with a silicone-based tape:
- Neonatal Epidermolysis Bullosa: A Clinical Practice Guideline
- This Clinical Practice Guideline has EB recommendations for skin care and management and medical care that overlaps with general EB care. Refer to Appendix 5 for the Neonatal EB Hospitalization Implementation with photographs of nasogastric tube securement.
Pre-Op Considerations
- For Dystrophic EB (DEB) & Junctional EB (JEB) - consider pre-op anemia screening
- For DEB, EB Simplex-Muscular Dystrophy, & EB Simplex with KLHL 24 mutation - check for recent ECHO
- Prepare for difficult intubation with ENT/ Pulmonary back-up
- Discuss operating room modifications with patients and/or families.
- Consider padding the operating room table with an egg crate to reduce pressure on the skin.
- Additional pieces of egg crate may need to be cut down to size for additional padding under straps, hard surfaces, or equipment for additional protection.
- For the use of electrocautery, consider a reusable pressure reducing bovie pad.
- Instruments encountering the skin should be lightly lubricated with an emollient to reduce friction, rubbing and skin trauma.
- If Betadine is applied to the surgical incision site, gently blot it away using a wound cleanser or sterile saline to help prevent irritation and itching.
- CCHMC Peri-operative Recommendations
- This includes Cincinnati Children’s Peri-operative Recommendations for preparation of an EB patient in Same Day Surgery, intra-op and post-anesthesia care
General Recommendations
- Listen to the family or adult patient
- Skin care is patient specific; tolerance varies and tailored interventions may be required
- Pad or lubricate any and all medical equipment in contact with the patient. For tubes that are in direct contact with the skin, lubricate with a petroleum-based lubricant such as Vaseline® petrolatum or Aquaphor® to minimize friction. For tubes that come into contact with the patient’ s mucosal surfaces, lubricate with water soluble lubricants
- Consider using gloves that are slippery (i.e. coated with petroleum- based lubricant) prior to handling the patient
- Dab, do not rub
- Generally, silicone-based products are well tolerated. Routine use of sutures and surgical glue if indicated
EB Emergency Wallet Card
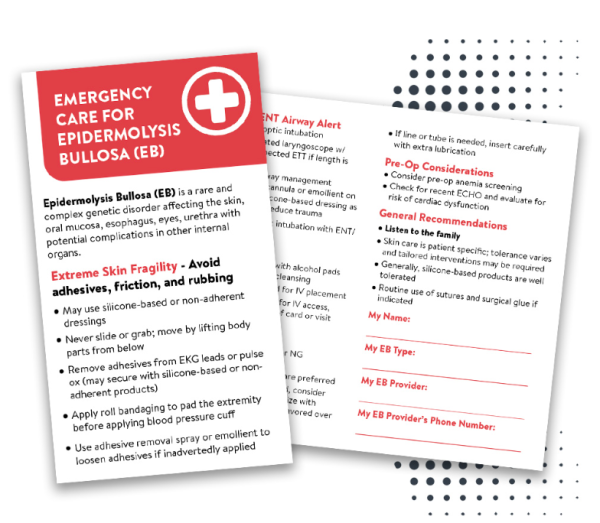
Alongside this comprehensive guide, we provide two essential tools: the EB Emergency Wallet Card and the EB Emergency Sticker.
The EB Emergency Wallet Card is a handy reference that consolidates crucial information for quick access. It includes key details that can help medical staff provide informed care during emergencies. Our EB Emergency Sticker, which features a QR code, can be placed in easily visible locations, giving instant access to this information, when you need it most.
Request your cards and stickers by submitting the form below to ensure you're always prepared. You may also print it on your own, here.
**United States Mailing Addresses Only. We are unable to send mail outside the United States.**
Request Your Free EB Emergency Wallet Card
More In-Depth Info for the ER
- DEBRA International’s Emergency Management Steps for EB
- This reference provides information regarding EB skin care management as well as the most common EB related prompts for seeking medical evaluation. These medical prompts includes clinical history, clinical features, healthcare provider evaluation and recommendations for treatment.
- Emergency Management in Epidermolysis Bullosa: Consensus Clinical Recommendations from the European Reference Network for Rare Skin Diseases
- This article thoroughly discusses the consensus clinical recommendation for emergency management in EB which is summarized by DEBRA International in the Emergency Management Steps of Epidermolysis Bullosa provided above.
- Caring for Pediatric Patients with Epidermolysis Bullosa in the Emergency Department
- This article includes a literature review and expert opinions regarding EB care in the emergency department. Refer to Table 1 in this article for quick reference recommendations for the below guideline topics addressed in this article:
- Approach to Patients with EB
- Bedding, Transferring and Patient Handling
- Adhesives and Adhesive Removal
- Monitoring Devices and Patient Identification
- Wound Dressings
- Wound Dressing Changes
- Assessing Wounds for Evidence of Infection
- Urinary Catheters
- Enteral Tubes
- Pain and Anxiety
- Pruritus
- Medication Administration
- Procedures
- Oxygenation & Intubation
- This article includes a literature review and expert opinions regarding EB care in the emergency department. Refer to Table 1 in this article for quick reference recommendations for the below guideline topics addressed in this article:
Acknowledgements
Contributors:
Catherine Doernbrack, CPNP, debra of America EB Nurse Educator & Children’s Hospital of Colorado
Beth Moeves, APRN-CNP, EB Nurse Practitioner at CCHMC
Caitin Treuting, Medical Photographer at CCHMC
Kalyani Marathe, MD, Dermatology Medical Director at CCHMC
Anne Lucky, MD, EB Medical Director at CCHMC
Lisa Remer, MD, EB Medical Director at CCHMC
Nichole Halliburton, APRN-CNP, EB Nurse Practitioner at CCHMC
Eric Wittkugel, MD, Anesthesiologist at CCHMC
Abigail Monnig, MD, Anesthesiologist at CCHMC
Ken Goldschneider, MD, Anesthesiologist at CCHMC
Katie Stephenson, RN at CCHMC
Jaime Webb, Vascular Access RN at CCHMC
Staff with CCHMC Perioperative Services
debra of America would like to extend our heartfelt thanks to these medical professionals for their invaluable contributions and expertise in reviewing this content.



